Screening and treatment for Osteoporosis
 Osteoporosis is a condition in which a person's bone mass is lost faster than it can be replaced. This results in bones that are weak, less dense and more likely to break. Osteoporosis s characterized by loss of bone and increased skeletal fragility, leading to an increased number of fractures. Osteoporosis is a condition in which a person's bone mass is lost faster than it can be replaced. This results in bones that are weak, less dense and more likely to break. Osteoporosis s characterized by loss of bone and increased skeletal fragility, leading to an increased number of fractures.
Ultrasound bone sonometry is a safe, radiation-free modality that provides precise quantitative assessment of skeletal status, useful in identifying patients at risk of developing osteoporosis and for assessing their risk of future fracture. The result takes less than a minute to be ready for interpretation by the rheumatologist.
Osteoporosis
Osteoporosis is a common bone disease that affects both men and women, usually as they grow older. Fortunately, you can take steps to reduce your risk of developing osteoporosis and avoid the often-debilitating bone fractures that can result from this disease. If you already have osteoporosis, new medications are available to slow or even stop its progression.
Fast facts
- Age is not the only risk factor for osteoporosis. Lifestyle choices, certain diseases and even medications can cause this condition.
- A simple diagnostic test known as a bone density test can provide valuable information about your bone strength.
- New medications exist to slow and even stop the progression of osteoporosis.
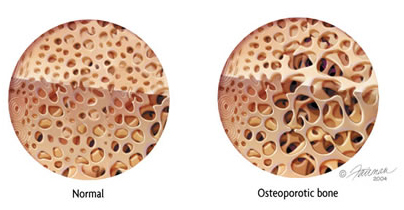
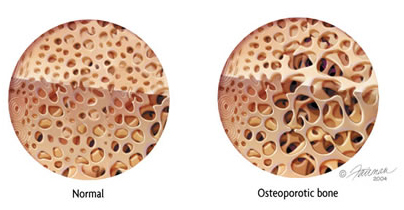
Osteoporosis is a condition of weak bone caused by a loss of bone mass as well as a change in bone structure. The first picture is normal bone and the second shows osteoporotic bone.
WHAT IS OSTEOPOROSIS?
Osteoporosis is a silent disease of the bones that makes them weaken and prone to fracture. Bone is living tissue that is in a constant state of regeneration, as old bone is removed (bone resorption) and replaced by new bone (bone formation). By their mid-30s, most people begin to gradually lose bone strength as the balance between bone resorption and bone formation shifts, so that more bone is lost than can be replaced. As a result, bones become thinner and structurally weaker.
The disease is silent because there are no symptoms when you have osteoporosis, and the condition may come to your attention only after you break a bone. When you have osteoporosis, this can occur even after a minor injury, such as a fall. The most common fractures occur at the spine, wrist and hip. Spine and hip fractures in particular may lead to chronic pain, long-term disability and even death. The goal of treating osteoporosis is to prevent such fractures in the first place.
WHAT CAUSES OSTEOPOROSIS?
Many factors will increase your risk of developing osteoporosis and suffering a fracture. Some of these risk factors can be changed, while others cannot. Recognizing your own risk factors is important so you can take steps to prevent this condition from developing or treat it before it becomes worse. Major risk factors include:
- Older age (starting in the mid-30s but accelerating with advancing age)
- Non-Hispanic white and Asian ethnic background
- Small bone structure
- Family history of osteoporosis or osteoporosis-related fracture in a parent or sibling
- Previous fracture following a low-level trauma, especially after age 50
- Sex hormone deficiency, particularly estrogen deficiency, both in women (e.g. menopause) and men
- Anorexia nervosa
- Cigarette smoking
- Alcohol abuse
- Low dietary intake or absorption of calcium and vitamin D
- Sedentary lifestyle or immobility
- Medications: glucocorticoid medications such as prednisone (Deltasone, Orasone, etc.), or prednisolone (Prelone) (see fact sheet on glucocorticoid-induced osteoporosis); excess thyroid hormone replacement; the blood thinner heparin (Calciparine, Liquaemin, etc.); certain anti-convulsant medications such as phenytoin (Dilantin),etc.
- Certain diseases can affect bone, such as endocrine disorders (hyperthyroidism, hyperparathyroidism, Cushing's disease, etc.) and inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, etc.)
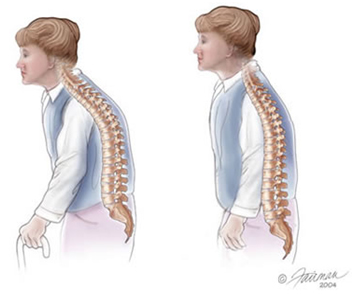
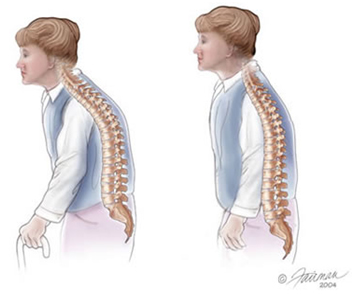
As the bone of the spine thins, factures can occur that cause a loss of height and a forward curvature of the spine.
Who gets osteoporosis?
Osteoporosis is more common in older individuals and non-Hispanic white women, but can occur at any age, in men as well as in woman, and in all ethnic groups.
In the U.S., about 8 million women and 2 million men have osteoporosis. Those over the age of 50 are at greatest risk of developing osteoporosis and suffering related fractures. In this age group, one in two women and one in six men will suffer an osteoporosis-related fracture at some point in their life. Non-Hispanic white and Asian people are most likely to experience osteoporosis and osteoporosis-related fractures. Hispanic and non-Hispanic black people also can develop osteoporosis and related fractures, but have a lower risk when compared to non-Hispanic whites and Asians.
How is osteoporosis diagnosed?
A simple test that measures bone mineral density (BMD)such as ultrasound bone sonometry BMD test which is a safe, radiation-free test that provides precise quantitative assessment of skeletal status, useful in identifying patients at risk of developing osteoporosis and for assessing their risk of future fracture.
The BMD score taken from the test is compared to the BMD of young, healthy individuals, resulting in a measurement called a T-score. Your bone density is considered normal if the T-score is between 1.0 and -1.0. If your T-score is –2.5 or lower, you are considered to have osteoporosis and, therefore, are at high risk for a fracture. T-scores between –1.0 and –2.5 are generally considered to show osteopenia. The risk of fractures generally is lower in people with osteopenia when compared with those with osteoporosis but, if bone loss continues, the risk for fracture increases.
How is osteoporosis treated?
To maintain bone health:
- Make sure there is enough calcium in your diet (1000 mg per day of calcium for adults under the age of 50 and 1200 mg per day for those ages 50 and older, which are the current recommended guidelines from the National Osteoporosis Foundation).
- Get adequate vitamin D intake, which is important for calcium absorption and to maintain muscle strength (400-800 IU per day for adults younger than age 50, 800 to 1000 IU per day for those age 50 and older, which are the current recommended guidelines from the National Osteoporosis Foundation). Doses may need to be adjusted according to blood levels of vitamin D.
- Get regular exercise, especially weight-bearing exercise.
A number of medications are also used for the prevention and treatment of osteoporosis:
- Bisphosphonates: Alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva) and zoledronic acid (Reclast) have been FDA-approved for the prevention and treatment of osteoporosis in postmenopausal women. Alendronate, risedronate, and zoledronic acid also have been approved for the treatment of osteoporosis in men and for the prevention and treatment of glucocorticoid-induced osteoporosis in both men and women. These medications help slow down bone loss and have been shown to decrease the risk of fractures. Alendronate, risedronate and ibandronate are pills that must be taken on an empty stomach with water only or else the medication won’t be absorbed properly. Because they have the potential for irritating the esophagus, remaining upright for at least an hour after taking these medications is recommended. Once-daily or once-weekly dosing is available for alendronate and risedronate, while once-monthly dosing is available for risedronate and ibandronate. Ibandronate also can be given through the vein (intravenous [IV]) every 3 months, while zoledronic acid is only available as an IV medication and is given once a year. There are other bisphosphonates available, etidronate (Didronel), pamidronate (Aredia) and tiludronate (Skelid), but they are not currently FDA approved for osteoporosis management.
There have been reports of jaw osteonecrosis (permanent bone damage of the bones of the jaw) resulting from high dose IV bisphosphonates used primarily in the management of people with underlying cancers. The risk for this problem in those taking these medications at doses recommended for osteoporosis management is not clearly established, but appears to be low.
In women who are considering future pregnancy or who are pregnant or breastfeeding, the risk to an unborn child from taking bisphosphonates is not well studied. Even if bisphosphonates are stopped, they can stay in the body a very long time. Animal studies show that bisphosphonates cross the placenta and enter fetal bone. The risk of harm to the developing fetus in humans is unknown, but theoretical. Thus, the anticipated benefits of bisphosphonates in women who want to become pregnant should be weighed against the potential risks. If a woman who previously has taken or is taking a bisphosphonate becomes pregnant, her blood calcium levels should be monitored carefully as they could become low.
- Calcitonin (Calcimar, Miacalcin): This medication, a hormone made from the thyroid gland, is given usually as a nasal spray or as an injection under the skin. It has been FDA approved for the management of postmenopausal osteoporosis and helps prevent vertebral (spine) fractures. It also is helpful in controlling pain after an osteoporotic vertebral fracture.
- Estrogen or Hormone Replacement Therapy: Estrogen therapy alone or in combination with another hormone, progestin, has been shown to decrease the risk of osteoporosis and osteoporotic fractures in women. However, the combination of estrogen with a progestin has been shown to increase the risk for breast cancer, strokes, heart attacks and blood clots. Estrogens alone may increase the risk of strokes. Given the complexity of this decision, consult with your doctor about whether hormone replacement therapy is appropriate for you.
- Selective Estrogen Receptor Modulators (SERMs): These medications mimic estrogen's good effects on bones without some of the serious side effects such as breast cancer. However, there is still a risk of blood clots and stroke with use of SERMs. Raloxifene (Evista) decreases spine fractures in women, and is approved for use only in post-menopausal women at this time.
- Bisphoshonates like Fosamax, Actonel(Taken once a week), Bonviva( Taken once a month) for prevention and treatment for osteoporosis.
- Strontium ranelate (Protelos): A powder dissolved in water and taken daily, this medication has been shown to reduce the risk for fractures in postmenopausal women. It is currently available in Europe, but not the USA. Because of an increased risk of blood clots, it should be used with caution in women who have a history or risk for deep venous thrombosis or pulmonary embolism.
- Teriparatide (Forteo or Forsteo): Teriparatide is a form of parathyroid hormone that helps stimulate bone formation. It is approved for use in postmenopausal women and men at high risk for osteoporotic fracture. It also is approved for treatment of glucocorticoid-induced osteoporosis. It is given as a daily injection under the skin and can be used for up to 2 years. If you have ever had radiation treatment or your parathyroid hormone levels are already too high, you may not be able to take this medication.
- Recently Denosumab (Prolia) 60mg sc injection given under the skin once every six months has been approved for the treatment for osteoporosis in postmenoausal women at increased risk of fracture and treatment of bone loss associated with hormone ablation in men with prostate cancer at increased risk of fractures.
Prevention
Lifestyle changes may be the best way of preventing osteoporosis:
- Make sure you are getting enough calcium in your diet (roughly 1000 to 1200 mg/day, but will depend on your age)
- Make sure you are getting enough vitamin D (between 400 to 1000 IU/day, depending on your age)
- Stop smoking
- Avoid excess alcohol intake
- Engage in weight-bearing exercises
- Treat underlying medical conditions that can cause osteoporosis
- Minimize or change medications that can cause osteoporosis; never stop taking any medication without speaking with your doctor first
- If you are at high risk for falls, consider using hip protectors (e.g. SAFEHIP ®), which may help prevent a hip fracture if you fall
Broader health impact of osteoporosis
The most health-threatening consequence of osteoporosis is a fracture. Spine and hip fractures especially may lead to chronic pain, long-term disability and even death. The major goal of treating osteoporosis is to prevent fractures.
Living with osteoporosis
If you have osteoporosis, it is important not only to help prevent further bone loss, but also to prevent a fracture. Eliminate hazards in the house that can increase your risk of falling (remove loose wires or throw rugs, install grab bars in the bathroom and non-skid mats near sinks and in the tub, etc.) Be careful when you are carrying or lifting items, as this could cause a spine fracture. Wear sturdy shoes, especially in winter. Use a cane or walker if you have balance problems or other difficulties walking.
Points to remember

Appropriate exercise is key in the treatment of osteoporosis.
- Make sure there is enough calcium and vitamin D in your diet.
- Get regular exercise.
- Eliminate lifestyle choices that increase your risk of osteoporosis.
The rheumatologist's role in the treatment of osteoporosis
As specialists in musculoskeletal diseases, rheumatologists can help to determine the cause of osteoporosis and can begin the treatment for osteoporosis.
To make an appointment for screening and treatment for osteoporosis, please contact the Rheumatology clinics at www.arthritisandpainclinic.com
|

 Osteoporosis is a condition in which a person's bone mass is lost faster than it can be replaced. This results in bones that are weak, less dense and more likely to break. Osteoporosis s characterized by loss of bone and increased skeletal fragility, leading to an increased number of fractures.
Osteoporosis is a condition in which a person's bone mass is lost faster than it can be replaced. This results in bones that are weak, less dense and more likely to break. Osteoporosis s characterized by loss of bone and increased skeletal fragility, leading to an increased number of fractures.